(Of 165 patients admitted to ICUs, 79 (48%) died. ) ---- NOTE:- There
are machines called FULL FEATURED VENTILATORS
SOURCE
a
study of Wuhan, China, are even grimmer. Only
3 of 22 ventilated patients survived.
Compare that to the 36% mortality rate of non-COVID
patients receiving advanced respiratory support.
Data from China, Italy and the U.S. suggest that about
half of those with covid-19 who receive
ventilator support will die.
Patients become severely confused and may have nightmarish hallucinations.
Even a year after leaving the intensive care unit, many people experience:
- post-traumatic stress disorder,
- Alzheimer’s-like cognitive deficits,
- depression,
- lost jobs and
- problems with daily activities such as bathing and eating.
source Washington Post
Many will suffer long-term physical, mental and
emotional issues, according to a staggering body of medical and
scientific studies. Even a year after leaving the intensive care unit,
many people experience post-traumatic stress disorder,
Alzheimer’s-like cognitive deficits, depression, lost jobs and
problems with daily activities such as bathing and eating.
Study of 18 ventilated patients in
Washington state found that nine were still alive when the study ended,
but only six had recovered
enough to breathe on their own.
All the early research suggests that once coronavirus patients are placed
on a ventilator, they will probably need to stay
on it for weeks. And the longer
patients remain on a breathing machine, the more
likely they are to die.
SOURCE NPR
Instead of quickly sedating people who had shockingly low levels of
oxygen and then putting them on mechanical ventilators,
many doctors are now keeping patients conscious, having them roll over in
bed, recline in chairs and continue to breathe on their own — with
additional oxygen — for as long as possible.
By Jim Dwyer April 14, 2020
SOURCE NYT

Some doctors have placed Covid-19 patients on special
massage mattresses made for pregnant women
because it has cutouts that ease the load on the belly and chest..
The idea is to get them off their backs and thereby make more lung
available. “Obesity is clearly a
critical risk factor.”
The first patient to rest on it arrived with
oxygen saturation in the 40s, breathing rapidly and with an
abnormally fast heartbeat, he said. After the patient was given
oxygen through a
nasal cannula — (clear plastic tubes that fit into the nostrils)
— Dr. Levitan helped her to lie face down on the
massage table. The oxygen
level in her blood climbed to the
mid-90s, he said, her pulse slowed to under
100 and she was breathing at a more normal pace. “She slept for two hours,”.
Other doctors are rejiggering CPAP
breathing machines, (normally used to help people with sleep apnea), or they
have hacked together valves and filters.
But for some critically ill patients,
a ventilator may
be the only real hope.
Many Covid-19 patients remain unusually alert,
even when their oxygen has sharply fallen, for reasons health
care workers can only guess. (Another important signal about how sick the
patients are — inflammatory markers in the
blood — is not available
until laboratory work is done.)
Some patients, by taking oxygen and rolling onto
their sides or on their bellies, have quickly returned to normal levels.
The tactic is called Proning.
There's a guide for patients on how often to turn themselves.
50 patients who arrived with low oxygen
levels between 69 and
85 percent (95 is normal).
After five minutes of
Proning, they had improved to a mean of 94
percent.
Over the next 24 hours, nearly 3/4 were
able to avoid intubation;
13 needed
ventilators.
Proning does not seem to
work as well in
older patients, a number of doctors said.
No one knows yet if this will be a lasting remedy, Dr. Caputo said, but if
he could go back to early March, he would advise himself and others: “Don’t jump to intubation.”
Contrary to expectations, a number of doctors at New York hospitals believe
intubation is helping
fewer people with Covid-19 than other respiratory illnesses and that longer
stays on the mechanical ventilators lead to other serious complications. The
matter is far from settled.
“Intubated patients with Covid lung disease are doing very poorly, and while
this may be the disease and not the mechanical ventilation, most of us
believe that intubation is to be avoided until
unequivocally required,” Dr. Strayer said.
" the risks of Proning were low. “This
is a simple technique which is safe and fairly easy to do,” Dr. Farkas said.
“I started doing this some years ago in
occasional patients, but never imagined that it would become this widespread
and useful.”
“I wouldn’t be surprised if in a couple of weeks someone around the country
comes up with better way to do this,” Dr. Swaminathan said.
SOURCE NYT
Covid-19 Does Not Lead to a “Typical” Acute Respiratory Distress
Syndrome? March 30, 2020
Luciano Gattinoni, Mattia Busana - Department of
Anesthesiology and Intensive Care Medicine, Medical University of Göttingen
Silvia Coppola, Davide Chiumello - Department of Anesthesiology and
Critical Care, San Paolo Hospital, University of Milan
Massimo Cressoni
- Department of Radiology, San Gerardo Hospital, University of Milan-Bicocca,
Correspondence:
gattinoniluciano@gmail.com
Dear Editor,
In northern Italy an overwhelming number of patients with Covid-19
pneumonia and acute respiratory failure have been admitted to our Intensive
Care Units.
Attention is primarily focused on increasing the number of beds, ventilators
and intensivists brought to bear on the problem, while the clinical approach
to these patients is the one typically applied to severe ARDS, namely high
Positive End Expiratory Pressure (PEEP) and prone positioning.
However, the patients with Covid-19 pneumonia, fulfilling the Berlin
criteria of ARDS, present an atypical form of the syndrome.
Indeed, the primary characteristics we are observing (confirmed by
colleagues in other hospitals), is the dissociation
between their relatively well preserved lung mechanics and the severity of
hypoxemia.
As shown in our first 16 patients
(Figure 1), the respiratory system compliance of 50.2 ± 14.3 ml/cmH2O is
associated with shunt fraction of 0.50 ± 0.11. 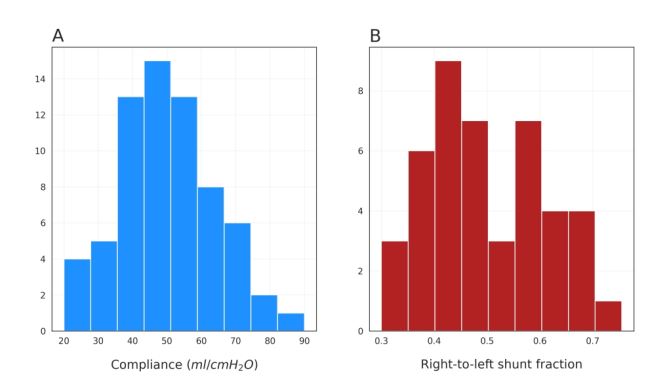
Figure 1
Such a wide discrepancy is virtually never seen in most forms of ARDS.
Relatively high compliance indicates well
preserved lung gas volume in this patient cohort, in sharp contrast to
expectations for severe ARDS.
A possible explanation for such severe hypoxemia occurring in compliant
lungs is the loss of lung perfusion regulation and hypoxic vasoconstriction.
Actually, in ARDS, the ratio between the shunt fraction to the fraction
of gasless tissue is highly variable, with mean 1.25 ± 0.80(1).
In eight of our patients with CT scan, however, we measured a ratio of
3.0 ± 2.1, suggesting remarkable hyperperfusion of gasless tissue.
If so, the oxygenation increases with high PEEP and/or prone position
are not primarily due to recruitment (keep open
otherwise collapsed lung regions), the usual mechanism in ARDS(2), but instead, in these patients with a
poorly recruitable pneumonia(3),
to the redistribution of perfusion (passage of
blood through the circulatory system or fluid thru lymphatic system to an
organ or a tissue) in response to pressure and/or gravitational
forces.
We should consider that:
- Patients treated with Continuous Positive Airway
Pressure or Non Invasive Ventilation, presenting with clinical signs of
excessive inspiratory efforts, intubation
should be prioritized to avoid excessive intrathoracic negative pressures
and self-inflicted lung injury(4).
- High PEEP
in a poorly recruitable lung tends to result in severe hemodynamic
impairment and fluid retention;
- Prone positioning of patients with relatively
high compliance results in a modest
benefit at the price of a high demand for stressed human resources.
After considering that, all we can do ventilating
these patients is “buying time” with minimum additional damage: the
lowest possible PEEP and gentle ventilation.
We need to be patient.
Bibliography
1. Cressoni M, Caironi P,
Polli F, Carlesso E, Chiumello D, Cadringher P, Quintel M, Ranieri VM,
Bugedo G, Gattinoni L.
Anatomical and functional intrapulmonary shunt in
acute respiratory distress syndrome.
Critical care medicine 2008. --- PubMed
Functional shunt poorly estimates the anatomical shunt compartment,
due to the large variability in apparent perfusion ratio.
Changes in anatomical shunt compartment with increasing positive
end-expiratory pressure, in each individual patient, may be estimated
from changes in functional shunt, only if the anatomical-functional
shunt relationship at 5 cm H2O positive end-expiratory pressure is known
The anatomical and
functional shunt conundrum: what do we really know about the
pathophysiology of acute respiratory distress syndrome? [Crit Care Med. 2008]
Anatomical and functional intrapulmonary
shunt in acute respiratory distress syndrome. [Crit Care Med. 2008]
Changes in anatomical shunt compartment with
increasing positive end-expiratory pressure, in each individual
patient, may be estimated from changes in functional shunt, only if
the anatomical-functional shunt relationship at 5 cm H2O positive
end-expiratory pressure is known.
Anatomical
intrapulmonary shunt. [Crit Care Med. 2008]
2. Gattinoni L, Caironi P,
Cressoni M, Chiumello D, Ranieri VM, Quintel M, Russo S, Patroniti N,
Cornejo R, Bugedo G.
Lung recruitment in patients with the acute
respiratory distress syndrome.
N Engl J Med 2006; 354: 1775-1786. --
PubMed --- NIH
In the acute respiratory distress syndrome (ARDS), positive
end-expiratory pressure (PEEP) may decrease ventilator-induced lung
injury by keeping lung regions open that otherwise would be collapsed.
Since the effects of PEEP probably depend on the recruitability of lung
tissue, we conducted a study to examine the relationship between the
percentage of potentially recruitable lung, as indicated by computed
tomography (CT), and the clinical and physiological effects of PEEP.
68 patients with acute lung
injury or ARDS underwent whole-lung CT during breath-holding sessions at
airway pressures of 5, 15, and 45 cm of water.
The percentage of potentially recruitable lung was defined as the
proportion of lung tissue in which aeration was restored at airway
pressures between 5 and 45 cm of water.
The percentage of potentially recruitable lung varied widely in the
population, accounting for a mean (+/-SD) of 13+/-11 percent of the lung
weight, and was highly correlated with the percentage of lung tissue in
which aeration was maintained after the application of PEEP (r2=0.72,
P<0.001).
On average, 24 percent of the lung could not be recruited.
Patients with a higher percentage of potentially recruitable lung
(greater than the median value of 9 percent) had
- greater total lung weights (P<0.001),
- poorer oxygenation (defined as a ratio of partial pressure of
arterial oxygen to fraction of inspired oxygen) (P<0.001) and
- respiratory-system compliance (P=0.002),
- higher levels of dead space (P=0.002), and
- higher rates of death (P=0.02)
than patients with a lower percentage of potentially recruitable
lung.
The combined physiological variables predicted, with a sensitivity of
71 percent and a specificity of 59 percent, whether a patient's
proportion of potentially recruitable lung was higher or lower than the
median.
In ARDS, the percentage of potentially recruitable lung is extremely
variable and is strongly associated with the response to PEEP.
3. Pan C, Chen L, Lu C,
Zhang W, Xia JA, Sklar MC, Du B, Brochard L, Qiu H.
Lung Recruitability in SARSCoV-2 Associated Acute
Respiratory Distress Syndrome: A Single-center, Observational Study.
Am J Respir Crit Care Med 2020. NIH
In ARDS, the percentage of potentially recruitable lung is extremely
variable and is strongly associated with the response to
PEEP.
"In conclusion, our data show that lung recruitability can be
assessed at the bedside even in a very constrained environment and is
low in our patients with COVID-19 induced ARDS. Alternating body
positioning improved recruitability. Our findings do not imply that all
patients with SARSCoV-2 associated ARDS were poorly recruitable, and
both the severity and management of these patients can remarkably differ
among regions. Instead, we think these findings might incite clinicians
to assess respiratory mechanics and lung recruitability in this
population."
Patients who did not receive prone positioning had poor lung
recruitability, while alternating supine (face upward) and prone
positioning was associated with increased lung recruitability.
SCIENCEDAILY --- YouTube
4. Brochard L, Slutsky A,
Pesenti A.
Mechanical Ventilation to Minimize Progression of Lung
Injury in Acute Respiratory Failure. Am J Respir Crit Care Med 2017;
195: 438-442. NIH
Mechanical ventilation is used to sustain life in patients with acute
respiratory failure.
A major concern in mechanically ventilated patients is the risk of
ventilator-induced lung injury, which is
partially prevented by lung-protective ventilation.
Spontaneously breathing, nonintubated patients with acute respiratory
failure may have a high respiratory drive and breathe with large tidal
volumes and potentially injurious transpulmonary
pressure swings.
In patients with existing lung injury, regional forces generated by
the respiratory muscles may lead to injurious effects on a regional
level.
In addition, the increase in transmural pulmonary vascular pressure
swings caused by inspiratory effort may worsen vascular leakage.
Recent data suggest that these patients may develop lung injury that
is similar to the ventilator-induced lung injury observed in
mechanically ventilated patients.
As such, we argue that application of a lung-protective ventilation,
today best applied with sedation and endotracheal intubation, might be
considered a prophylactic therapy, rather than just a supportive
therapy, to minimize the progression of lung injury from a form of
patient self-inflicted lung injury.
This has important implications for the management of these patients.
AJRCCM Articles in Press. Published March 30, 2020 as
10.1164/rccm.202003-0817LE Copyright © 2020 by the
American Thoracic Society
SOURCE |
|
NOTE: Enzymes in the liver, include:-
- alanine transaminase (ALT),
- aspartate transaminase (AST),
- alkaline phosphatase (ALP), and
- gamma-glutamyl transpeptidase (GGT).
Elevated liver enzymes, found with a blood test, indicate inflamed or
injured liver cells.
Aspartate aminotransferase (AST) is an
enzyme found in cells throughout the body but mostly in the
heart and liver
and, to a lesser extent, in the kidneys and muscles.
In healthy individuals, levels of AST in the blood are low. When liver or
muscle cells are injured, they release AST into the blood
CPAP vs BPAP vs Ventilator
Medical professionals say people who use a
CPAP to treat
sleep apnea need to consult with a doctor if they contract
coronavirus,
because the risks of continuing to use the device may outweigh the
benefits.
- CPAPs are simpler devices than
ventilators. They produce a constant pressure, not the breath-to-breath
changes in pressure needed to push air into the lungs.
CPAPs typically don’t have audible
warning alarms. "If the power goes out, or if the patient stops breathing,
it doesn’t tell the medical staff.
But the bigger problem is that, unless they have been retrofitted,
CPAPs send out the user’s exhaled breaths
into the air. If a CPAP user is
infected, that releases the coronavirus widely.
"The air leaving the patient actually goes into the environment without
being filtered,"
- Ventilators are connected to tubes
that go into the patient's breathing passage itself, rather than just to
the mask. Ventilators also supply
oxygen, which CPAPs ordinarily don’t. And generally, ventilators have much
more sophisticated electronics for monitoring than
CPAPs do.
- A bilevel positive airway pressure
machine, or BIPAP, which works more
like a real ventilator in some ways.
While CPAP has the same pressure level
for inhalation and expiration, a BIPAP
has higher pressure for inhalation and lower pressure for exhalation.
If a BIPAP machine is modified to
filter out viruses, it can hold a patient who isn’t facing a severe case,
at least for a couple of days — possibly enough for a
ventilator to become available
SOURCE
https://www.politifact.com/article/2020/apr/08/how-useful-are-cpap-machines-during-ventilator-sho/
|